Get it right, make it safe.
Every 17 September, World Patient Safety Day reminds our industry that safety is not just an outcome it’s a discipline. In clinical research, safety begins long before first-patient-in and continues with every data point captured, every deviation resolved, and every monitoring decision made.
Start where safety starts: design
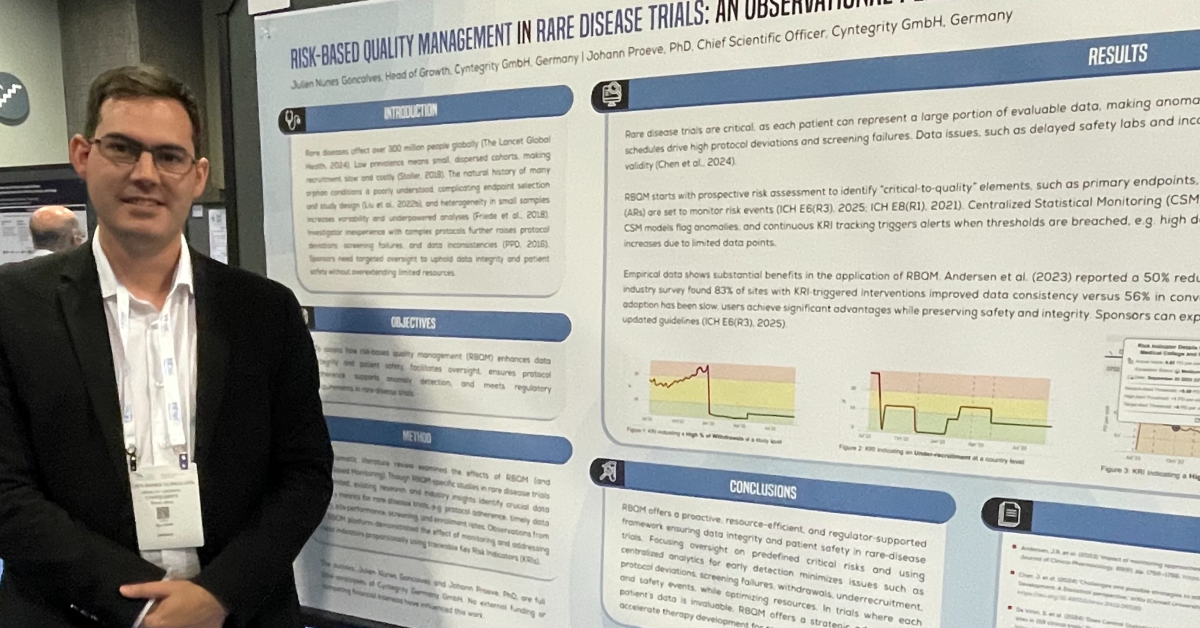
Picture the study team at protocol draft v0.7. The endpoints look achievable, but visit cadence, lab panels, and edit-check density risk unintended burden for patients and sites. This is where Quality by Design (QbD) and Risk-Based Quality Management (RBQM) act in concert:
- QbD shapes a protocol that is fit for purpose minimizing unnecessary procedures and complexity that add burden without adding value.
- RBQM anticipates where and how risks to patient safety and data integrity could emerge across the study lifecycle.
Cyntegrity operationalizes this hand-in-glove approach with its AI-augmented Protocol Complexity Analysis, quantifying the real load on participants and sites while exposing risk hot-spots early. The output feeds your risk assessment (RACT) and planning in the MyRBQM® ecosystem, so teams can right-size procedures, define Quality Tolerance Limits (QTLs), and lock in proactive controls before the first patient is enrolled. Learn more about structured risk assessment here: (Risk Assessment in Clinical Trials (RACT))
Impact: less avoidable burden (QbD), clearer critical-to-quality factors (RBQM), and a protocol that supports not strains patient safety from day one.
Keep safety visible: oversight that scales
Once the study is live, safety depends on timely signal detection and context. Static listings and broad SDV percentages rarely surface what matters most. Cyntegrity’s AI-enhanced Subject Profiles bring each participant’s journey into focus longitudinally, across data domains so medical monitors can act with confidence.
Subject Profiles help teams:
- See patient-level risk patterns early (e.g., AE clusters after titration, dose interruptions, lab drifts tied to concomitant meds).
- Investigate outliers and suspected duplicates quickly, reducing the time from “something looks off” to “we know why.
- Prioritize monitoring actions against QTLs and KRIs, aligning medical judgment with risk signals instead of volume.
Explore how medical monitoring teams use these capabilities: (Medical Monitoring for Clinical Trials)
Why this matters for patient safety
Safety isn’t a single control it’s an operating model:
- Design for safety (QbD): quantify complexity and remove non-value-adding procedures that create burden and dropout risk.
- Plan for risk (RBQM): perform structured risk assessment (RACT), set QTLs, and define proportionate controls.
- Monitor what matters: use predictive analytics and Subject Profiles to keep the patient not just the datapoint at the center of oversight.
Cyntegrity’s MyRBQM® Portal brings these steps together with real-time risk detection, predictive analytics, and medical-monitoring workflows. The platform also carries Microsoft Healthcare AI Certification, supporting confidence in safety, design, and performance for regulated use.
A practical call to action
- If you’re drafting or amending a protocol, run AI-augmented Protocol Complexity Analysis and close the loop with RACT lock in QTLs and burden-reducing changes before FPI.
Start here: Risk Assessment (RACT) - If your team is already live, enable AI-enhanced Subject Profiles to sharpen medical monitoring and accelerate issue resolution tied to patient risk.
See how: Medical Monitoring
Bottom line: Patient safety is won at two moments when you design the work, and when you decide what to do next. QbD plus RBQM, powered by Cyntegrity’s AI-augmented tools, gives study teams the clarity to do both.