Do current vaccines work against new coronavirus strains?
As evidence grows that variants of the SARS-CoV-2 coronavirus can evade immunity produced by vaccines or previous infections, clinical researchers are exploring the idea of redesigning the vaccines currently being rolled out worldwide. EMA’s latest guidance published on 26 February is for manufacturers that make coronavirus vaccines as they work to keep up with evolving variants of SARS-CoV-2.
The purpose of the reflection paper is to simplify the development and mitigate any unnecessary burden from the clinical organizations ensuring vaccines are readily available when needed.
The CHMP proposes different types of clinical studies:
On-top variant vaccine – After primary vaccination with the variant vaccine*; and after a single dose of the variant vaccine when given to subjects who previously received primary vaccination with the parent vaccine**.
Two vaccines in one shot – The variant vaccine is intended to replace the parent vaccine as the sole marketed vaccine and/or the variant vaccine will include the parent strain, i.e. it will consist of one or more variant strains plus the parent strain.
It is currently recommended that at least one trial should be conducted in a SARS-CoV-2-naïve population (which means no infection with any variant or parent strain of SARS-CoV-2), randomized to either the parent strain vaccination or the variant strain vaccination.
The seroconversion of the variant strain vaccination should not be below -10 % of the seroconversion observed in the parent strain vaccinated group. If the provision of parent strain vaccination is not indicated anymore (since the parent strain is not around anymore) then a historic comparison of the variant strain efficacy with the historic data of the parent strain efficacy can be performed.
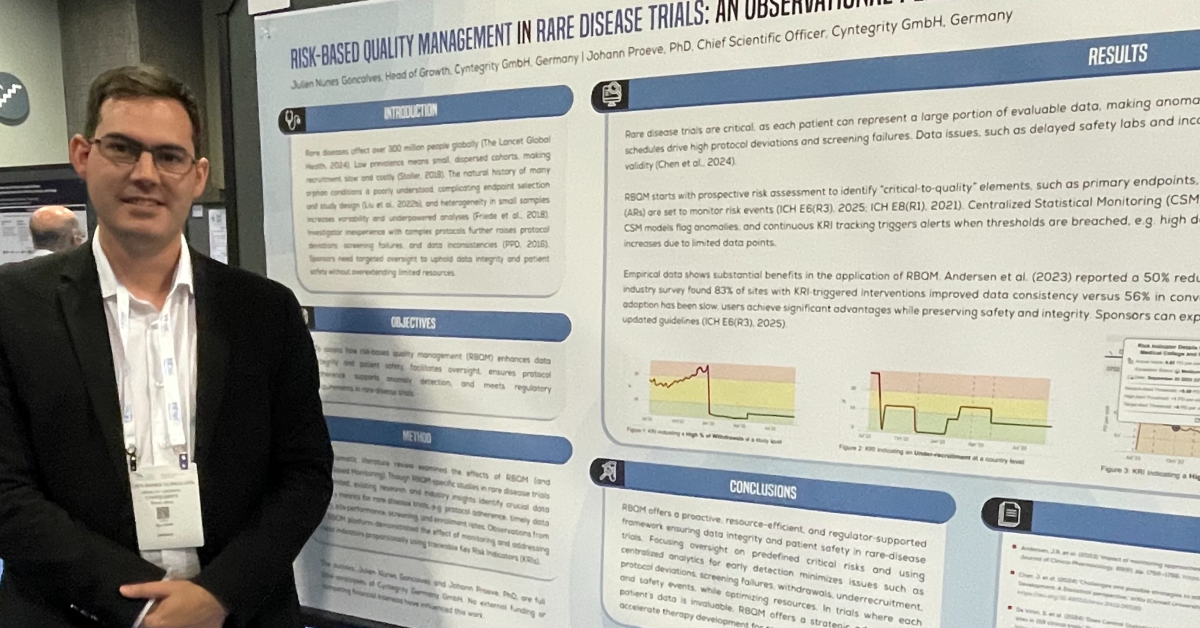
How can risk-based quality management (RBQM) help optimize these studies?
Below we outline four risk-based ways to optimize vaccine trials that target coronavirus (SARS-CoV-2) variants:
- On an ongoing basis, compare the seroconversion between the two treatment groups, either unblinded or in a blinded fashion by a trusted third party. This will permit an early termination in case of gross deviations of the parent and the variant strain efficacy, or, vice versa provide trust in the comparable efficacy of both vaccines.
- Reduce the source data verification since the safety profile of the parent strain vaccine is already known quite well. Focus can be put on a continuous comparison of both vaccine schemes with respect to pre-selected safety parameters.
- Use centralized statistical monitoring for the detection of any unexpected differences in the data between the two vaccines.
- Use key performance indicators to always be on top of the status of the trials, such as enrollment, data entry, query management, and patient completion. This will facilitate a timely database closure once the last subjects completed their last visits.
*Vaccines that are intended to protect against one or more SARS-CoV-2 variants that have emerged are referred to as variant vaccines and the SARS-CoV-2 strain(s) from which they are derived is/are designated as the variant strain(s).
**The original licensed vaccines against SARS-CoV-2 are referred to as parent vaccines and the SARS-CoV-2 strain from which they were derived is designated as the parent strain.
Download reflection paper: Reflection paper on the regulatory requirements for vaccines intended to provide protection against variant strain(s) of SARS-CoV-2